Tailored Drug Cocktails Offer Hope to Kids with Aggressive Brain Tumors
Tailored Drug Cocktails Offer Hope to Kids with Aggressive Brain Tumors
Clinical Trial Tests Personalized Treatments in Push to Improve Pediatric Cancer Survival
By Suzanne Leigh on August 29, 2018
UCSF Benioff Children’s Hospitals are harnessing next-generation genomic technology to develop individualized drug cocktails in a new trial for children with a type of malignant brain tumor. This precision-medicine approach offers a new strategy in the treatment for high-grade glioma, an intractable brain cancer in which survival has plateaued for decades.
In the trial, UCSF Health neuro-oncologist Sabine Mueller, MD, PhD, and her colleagues in the Pacific Pediatric Neuro-Oncology Consortium (PNOC) will treat up to 44 children and young adults. Patients will be enrolled at UCSF Benioff Children’s Hospital San Francisco and other sites in the 18-hospital PNOC network, which is tasked with translating new findings in cancer biology to more effective therapies.
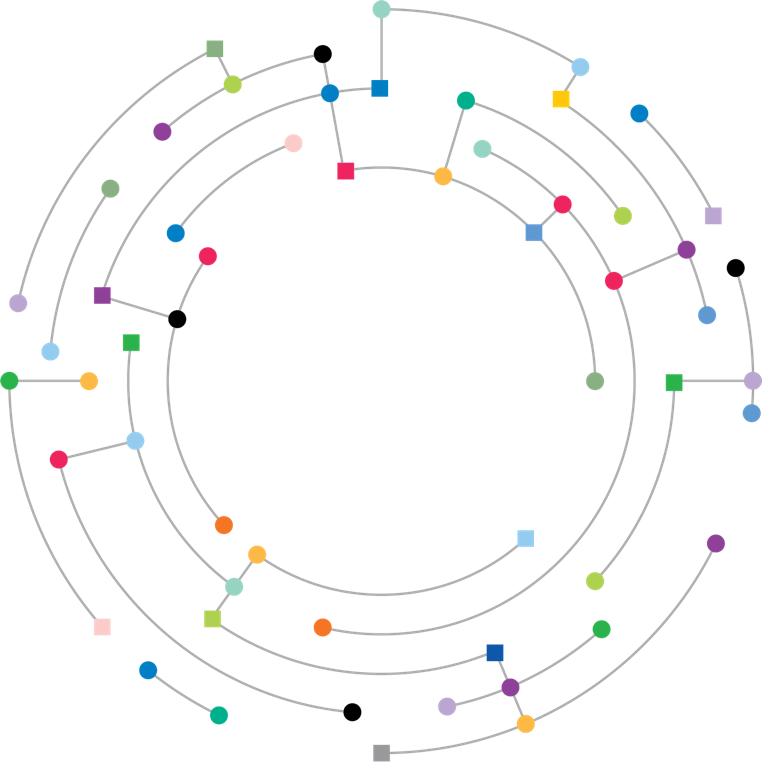
The drug cocktails will be developed with up to four therapies specifically targeted to the child’s tumor. Each will be screened using the UCSF 500 Cancer Gene Panel, which flags the most common cancer genetic mutations; and molecular profiling and analysis services provided by NantHealth, Inc. (NASDAQ: NH), which includes whole-genome and whole-exome sequencing for all DNA and genes, detecting any changes that promote cancer growth; as well as RNA sequencing, which offers important clues about the cancer gene expression and gene fusions that drive cancer progression.
The trial will be offered for patients with high-grade glioma that includes anaplastic astrocytoma, glioblastoma and midline high-grade glioma, all of which are aggressive forms of brain tumor with few current therapeutic options.
“While survival for some childhood cancers has been improving since the 1970s, this has not happened for some solid tumors, including types of pediatric brain tumors,” said Mueller, who is the project leader for PNOC.
“We have learned a lot about the molecular makeup of high-grade gliomas in recent years and we recognize that their heterogeneity means that a blanket treatment approach fails to reach most patients,” she said. “We hope that this personalized strategy may lead the way to life-saving treatments for children with high-grade gliomas, as well as other treatment-resistant brain tumors.”
Approximately 10 percent of the 4,610 tumors of the brain and central nervous system diagnosed each year in U.S. children and teens are high-grade gliomas, with two-year survival ranging from about 35 percent to less than 10 percent, Mueller said. While surgical techniques for brain tumors have improved over the years, some high-grade gliomas are inoperable or cannot be totally removed. Chemotherapy and radiation may extend survival. Medical services providing gamma knife radiosurgery or similar treatment can help to destroy the cancerous cells. But in some cases, the tumors remain resistant to long-term remission.
Standard Therapy Not Effective for Curbing Disease
Typically, when a child with high-grade glioma experiences tumor growth or recurrence, oncologists may propose different chemotherapy agents or re-irradiation following surgery, Mueller said, “But these therapies may be incompatible with the tumor’s unique biology and may do nothing to curb disease, while causing debilitating side effects.”
In the trial, researchers will analyze samples of tumor in a specialized lab and “read” the genetic makeup of both the tumor and normal cells using a DNA sequencer. Any genetic alterations may be matched with existing targeted therapies or investigational new drug study agents that block the growth of cancer by interfering with the molecular targets that drive progression.
“One of the pitfalls in identifying the drugs best suited for each child is that many therapies fail to cross the blood-brain barrier or have a high enough concentration to cause a biological effect,” said Michael Prados, MD, a neuro-oncologist at UCSF Benioff Children’s Hospitals and founder and co-project leader of PNOC.
“We are working with drugs that have demonstrated blood-brain barrier penetration, based upon laboratory findings or prior clinical studies,” Prados said. “However, anticipating delivery across the blood-brain barrier is different than actually knowing its impact in an individual patient. UCSF Benioff Children’s Hospitals, together with PNOC, will be studying this further in an upcoming trial.”
Scientists also will examine the DNA sequence in healthy cells to see if there are germline or heritable mutations that increase the risk for other cancers.
“We are pleased that the molecular profiling and analysis technology that drives our GPS Cancer product will be used to support important research in pediatric brain cancer,” said Patrick Soon-Shiong, MD, chairman and CEO of NantHealth. “By sequencing the entire genome, this technology ensures the most comprehensive and actionable data about the biology of the tumor will be available to the oncologist before treatment begins. The application in this study is of particular interest because there are generally fewer DNA mutations in pediatric cancers than in adult variations.”
A parallel trial is underway at UCSF Benioff Children’s Hospital San Francisco and other PNOC sites for children with the most virulent high-grade glioma, known as diffuse intrinsic pontine glioma (DIPG), using a similar precision medicine approach. Despite decades of research, the average survival for DIPG is less than one year.
Full article via UCSF.edu.