Research Findings on the Connection Between Obesity and Cancer

There are many benefits of living a healthy lifestyle: boosts your energy, improves your mood, and combats diseases. Living, and maintaining, a healthy lifestyle can also prevent weight gain. Healthy habits, such as keeping active and eating healthy, can help you maintain a healthy weight.
What does this have to do with cancer?
Being overweight or obese can lead to a number of conditions. Individuals with an unhealthy amount of body fat are at a higher risk of developing heart disease, diabetes, and some types of cancers.
It’s important that you know your body mass index (BMI) and the risks that affect those in the overweight (25.-29.9 BMI) and obese (30+ BMI) categories. You can calculate your BMI here. Visit your doctor for an accurate BMI assessment and to discuss potential lifestyle changes you can make to improve your health.
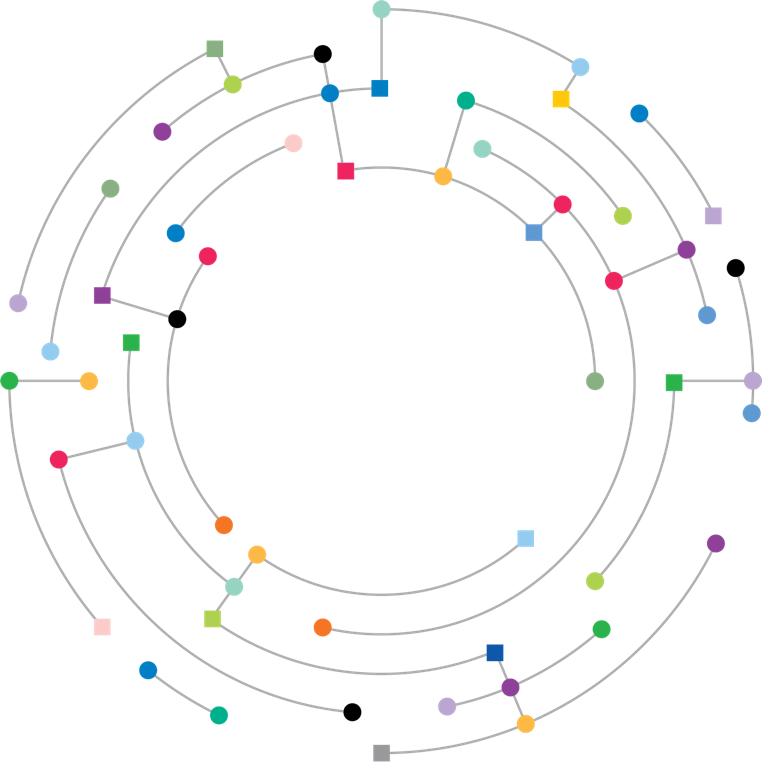
Obesity and Cancer
Source: cancer.gov
What is known about the relationship between obesity and cancer?
Nearly all of the evidence linking obesity to cancer risk comes from large cohort studies, a type of observational study. However, data from observational studies can be difficult to interpret and cannot definitively establish that obesity causes cancer. That is because obese or overweight people may differ from lean people in ways other than their body fat, and it is possible that these other differences—rather than their body fat—are what explains their different cancer risk.
Despite the limitations of the study designs, there is consistent evidence that higher amounts of body fat are associated with increased risks of a number of cancers (6), including:
- Endometrial cancer: Obese and overweight women are two to about four times as likely as normal-weight women to develop endometrial cancer (cancer of the lining of the uterus), and extremely obese women are about seven times as likely to develop the more common of the two main types of this cancer (7). The risk of endometrial cancer increases with increasing weight gain in adulthood, particularly among women who have never used menopausal hormone therapy (8).
- Esophageal adenocarcinoma: People who are overweight or obese are about twice as likely as normal-weight people to develop a type of esophageal cancer called esophageal adenocarcinoma, and people who are extremely obese are more than four times as likely (9).
- Gastric cardia cancer: People who are obese are nearly twice as likely as normal-weight people to develop cancer in the upper part of the stomach, that is, the part that is closest to the esophagus (10).
- Liver cancer: People who are overweight or obese are up to twice as likely as normal-weight people to develop liver cancer. The association between overweight/obesity and liver cancer is stronger in men than women (11, 12).
- Kidney cancer: People who are overweight or obese are nearly twice as likely as normal-weight people to develop renal cell cancer, the most common form of kidney cancer (13). The association of renal cell cancer with obesity is independent of its association with high blood pressure, a known risk factor for kidney cancer (14).
- Multiple myeloma: Compared with normal-weight individuals, overweight and obese individuals have a slight (10% to 20%) increase in the risk of developing multiple myeloma (15).
- Meningioma: The risk of this slow-growing brain tumor that arises in the membranes surrounding the brain and the spinal cord is increased by about 50% in people who are obese and about 20% in people who are overweight (16).
- Pancreatic cancer: People who are overweight or obese are about 1.5 times as likely to develop pancreatic cancer as normal-weight people (17).
- Colorectal cancer: People who are obese are slightly (about 30%) more likely to develop colorectal cancer than normal-weight people (18). A higher BMI is associated with increased risks of colon and rectal cancers in both men and in women, but the increases are higher in men than in women (18).
- Gallbladder cancer: Compared with normal-weight people, people who are overweight have a slight (about 20%) increase in risk of gallbladder cancer, and people who are obese have a 60% increase in risk of gallbladder cancer (19, 20). The risk increase is greater in women than men.
- Breast cancer: Many studies have shown that, in postmenopausal women, a higher BMI is associated with a modest increase in risk of breast cancer. For example, a 5-unit increase in BMI is associated with a 12% increase in risk (21). Among postmenopausal women, those who are obese have a 20% to 40% increase in risk of developing breast cancer compared with normal-weight women (22). The higher risks are seen mainly in women who have never used menopausal hormone therapy and for tumors that express hormone receptors. Obesity is also a risk factor for breast cancer in men (23). In premenopausal women, by contrast, overweight and obesity have been found to be associated with a 20% decreased risk of breast tumors that express hormone receptors (22).
- Ovarian cancer: Higher BMI is associated with a slight increase in the risk of ovarian cancer, particularly in women who have never used menopausal hormone therapy (24). For example, a 5-unit increase in BMI is associated with a 10% increase in risk among women who have never used menopausal hormone therapy (24).
- Thyroid cancer: Higher BMI (specifically, a 5-unit increase in BMI) is associated with a slight (10%) increase in the risk of thyroid cancer (25).
How might obesity increase the risk of cancer?
Several possible mechanisms have been suggested to explain how obesity might increase the risks of some cancers.
- Obese people often have chronic low-level inflammation, which can, over time, cause DNA damage that leads to cancer. Overweight and obese individuals are more likely than normal-weight individuals to have conditions or disorders that are linked to or that cause chronic local inflammation and that are risk factors for certain cancers (26). For example, chronic local inflammation induced by gastroesophageal reflux disease or Barrett esophagus is a likely cause of esophageal adenocarcinoma. Obesity is a risk factor for gallstones, a condition characterized by chronic gallbladder inflammation, and a history of gallstones is a strong risk factor for gallbladder cancer (27). Chronic ulcerative colitis (a chronic inflammatory condition) and hepatitis (a disease of the liver causing inflammation) are risk factors for different types of liver cancer (28).
- Fat tissue (also called adipose tissue) produces excess amounts of estrogen, high levels of which have been associated with increased risks of breast, endometrial, ovarian, and some other cancers.
- Obese people often have increased blood levels of insulin and insulin-like growth factor-1 (IGF-1). (This condition, known as hyperinsulinemia or insulin resistance, precedes the development of type 2 diabetes.) High levels of insulin and IGF-1 may promote the development of colon, kidney, prostate, and endometrial cancers (29).
- Fat cells produce adipokines, hormones that may stimulate or inhibit cell growth. For example, the level of an adipokine called leptin, which seems to promote cell proliferation, in the blood increases with increasing body fat. And another adipokine, adiponectin—which is less abundant in obese people than in those of normal weight—may have antiproliferative effects.
- Fat cells may also have direct and indirect effects on other cell growth regulators, including mammalian target of rapamycin (mTOR) and AMP-activated protein kinase.
Other possible mechanisms by which obesity could affect cancer risk include changes in the mechanical properties of the scaffolding that surrounds breast cells (30) and altered immune responses, effects on the nuclear factor kappa beta system, and oxidative stress (31).
A full list of references as well as more information on obesity and cancer can be found here.
It’s not too late to make a healthy change! Make a commitment to introduce a new healthy habit into your life this week